Cedars-Sinai Neonatal Intensive Care Unit, part of the Maxine Dunitz Children’s Health Center, is using new devices to personalise the nutritional care of premature babies for more rapid and healthier weight gain. In addition to improving nutrition, Cedars-Sinai is also using new specially designed mattresses to help improve sleep patterns and head shape development in preemies.
A device known as the Pea Pod, which resembles a miniature MRI machine, is used to measure the body composition of the infants. The Pea Pod is heated and the baby is placed inside for about three minutes. Using an air displacement method, the machine senses change in pressure and can determine the percentage of body weight that is fat and the percentage that is lean body mass. With this information, the NICU team can then personalise the baby’s nutritional supplements to help with proper weight gain.
“The Pea Pod is important in helping the NICU team facilitate a healthy weight gain in the smallest infants by calculating the amount of lean mass and body fat in the infant on a daily or weekly basis,” said Charles Simmons, MD, Chair of the Department of Pediatrics and Director of the Division of Neonatology. There are several units of the Pea Pod in use around the US and throughout the world.
Also, Cedars-Sinai is continuing a study of breast milk composition, utilising a device that analyses the percentages of fat, protein and carbohydrates in breast milk. To date, the research team has performed hundreds of analyses of breast milk.
The information from both analyses should ultimately lead to healthier weight gain, better neurological outcomes and shorter hospital stays for babies in the neonatal intensive care unit, according to Dr. Simmons, the Ruth and Harry Roman Chair in Neonatology, a position created in honour of Larry Baum.
New Mattress Helps with Head Shape and Sleep Cycles
The mattress, known as Lifenest, has oval-shaped netting in the centre and is intended to reduce pressure on different parts of the infant’s body including the head. Cedars-Sinai is currently the only hospital in the US with the new technologically advanced mattresses.
Since the 1990s, when babies were placed on their backs to reduce the risk of sudden infant death syndrome, the incidence of plagiocephaly – commonly known as flat head – has risen dramatically.
“We are interested in these mattresses because with the lower surface tension we expect less risk of head flattening and less risk for pressure ulcers,” said Ellen Mack, RNC, MN, neonatal clinical nurse specialist. The babies are constantly evaluated to determine if they are sleeping well and the infants seem to be comfortable with the new mattresses, she added.
“Together, these new technologies are helping us reduce the babies’ stay in the NICU and sending them home to their families, where they belong,” Dr. Simmons noted.
Equipment in the NICU
These devices are often used while a baby is in the NICU (neonatal intensive care unit):
- Incubator. This is the clear plexiglass box that makes up your baby’s bed. This enclosed space protects the baby from temperature changes. A radiant warmer over the bed may be used instead of an incubator to keep the baby warm. A cloth cover can be placed over an incubator to keep out noise and light.
- Cardiorespiratory monitor. This keeps track of the baby’s heartbeat and breathing. It’s attached to the baby’s skin with 3 leads (sensors). These are held in place with a gel that’s gentle to the skin.
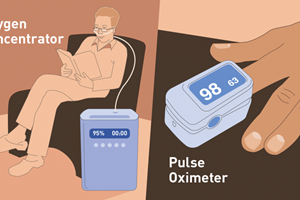
- Pulse oximeter. This measures the level of oxygen (called oxygen saturation) in the baby’s blood. It’s attached to the skin with a sensor taped to the baby’s hand or foot. It works by shining a light through the baby’s hand or foot.
- Blood pressure monitor. This may be a smaller version of the blood pressure cuff used on older children and adults. Or an arterial catheter (tiny tube inserted in an artery) may be used to monitor blood pressure.
- Temperature probe. This measures the baby’s body temperature. It’s attached to the skin surface.
- IV (intravenous) line. This is a small, flexible tube (catheter) inserted into a vein. It’s used to give the baby fluids, nutrition, and medicines.
- Umbilical arterial catheter (UAC) or umbilical venous catheter (UVC). This tube is placed in the artery or vein at the stump of the umbilical cord. It’s used to give the baby medicines, fluids, and nutrition. It’s also used to draw blood for lab tests. Because there are no pain nerves in the umbilical cord, putting the line in and maintaining it causes the baby no pain. But there is a higher risk of complications with an umbilical catheter than with an IV.
Other devices you may see
- Feeding tube (gavage tube). This goes through the mouth or nose into the stomach. It's used to feed the baby milk or formula.
- CPAP (continuous positive airway pressure) machine. This delivers air or oxygen through tubes in the nostrils. It uses low, continuous pressure to keep the lungs inflated.
- Endotracheal tube (ETT). This goes through the baby's mouth or nose into the windpipe. It's used with a respirator or ventilator to send air directly to the lungs.
- Respirator or ventilator. These machines may be used to help the baby breathe. They are attached to an ETT.
- Peripherally inserted central catheter (PICC) or a percutaneous central venous catheter (PCVC). This tube may be inserted in a central (large) vein. It's used to give the baby fluids, nutrition, and medicine.