Each year, more than 2.8 million people in the United States develop bacterial infections that don’t respond to treatment and sometimes turn life-threatening [1]. Their infections are antibiotic-resistant, meaning the bacteria have changed in ways that allow them to withstand our current widely used arsenal of antibiotics. It’s a serious and growing health-care problem here and around the world. To fight back, doctors desperately need new antibiotics, including novel classes of drugs that bacteria haven’t seen and developed ways to resist.
Developing new antibiotics, however, involves much time, research, and expense. It’s also fraught with false leads. That’s why some researchers have turned to harnessing the predictive power of artificial intelligence (AI) in hopes of selecting the most promising leads faster and with greater precision.
It’s a potentially paradigm-shifting development in drug discovery, and a recent NIH-funded study, published in the journal Molecular Systems Biology, demonstrates AI’s potential to streamline the process of selecting future antibiotics [2]. The results are also a bit sobering. They highlight the current limitations of one promising AI approach, showing that further refinement will still be needed to maximize its predictive capabilities.
These findings come from the lab of James Collins, Massachusetts Institute of Technology (MIT), Cambridge, and his recently launched Antibiotics-AI Project . His audacious goal is to develop seven new classes of antibiotics to treat seven of the world’s deadliest bacterial pathogens in just seven years. What makes this project so bold is that only two new classes of antibiotics have reached the market in the last 50 years!
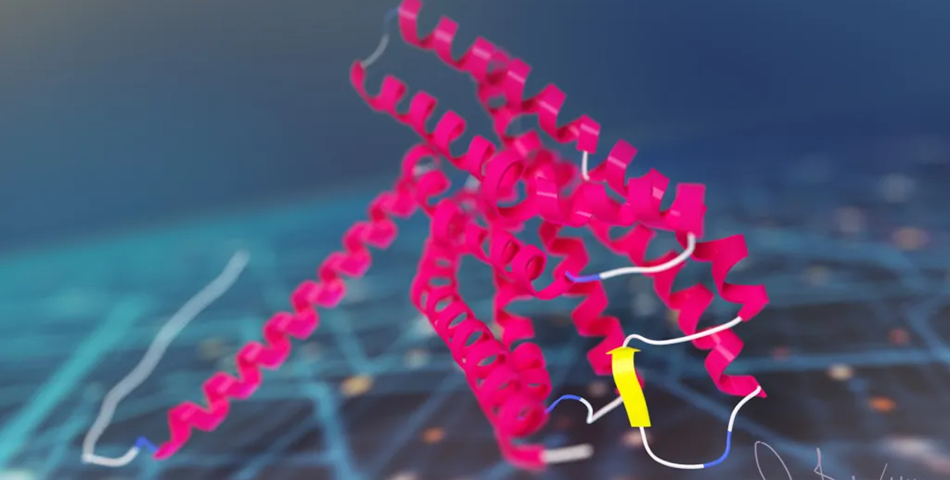
In the latest study, Collins and his team looked to an AI program called AlphaFold2 [3]. The name might ring a bell. AlphaFold’s AI-powered ability to predict protein structures was a finalist in Science Magazine’s 2020 Breakthrough of the Year. In fact, AlphaFold has been used already to predict the structures of more than 200 million proteins, or almost every known protein on the planet [4].
AlphaFold employs a deep learning approach that can predict most protein structures from their amino acid sequences about as well as more costly and time-consuming protein-mapping techniques.
In the deep learning models used to predict protein structure, computers are “trained” on existing data. As computers “learn” to understand complex relationships within the training material, they develop a model that can then be applied for making predictions of 3D protein structures from linear amino acid sequences without relying on new experiments in the lab.
Collins and his team hoped to combine AlphaFold with computer simulations commonly used in drug discovery as a way to predict interactions between essential bacterial proteins and antibacterial compounds. If it worked, researchers could then conduct virtual rapid screens of millions of new synthetic drug compounds targeting key bacterial proteins that existing antibiotics don’t. It would also enable the rapid development of antibiotics that work in novel ways, exactly what doctors need to treat antibiotic-resistant infections.
To test the strategy, Collins and his team focused first on the predicted structures of 296 essential proteins from the Escherichia coli bacterium as well as 218 antibacterial compounds. Their computer simulations then predicted how strongly any two molecules (essential protein and antibacterial) would bind together based on their shapes and physical properties.
It turned out that screening many antibacterial compounds against many potential targets in E. coli led to inaccurate predictions. For example, when comparing their computational predictions with actual interactions for 12 essential proteins measured in the lab, they found that their simulated model had about a 50:50 chance of being right. In other words, it couldn’t identify true interactions between drugs and proteins any better than random guessing.
They suspect one reason for their model’s poor performance is that the protein structures used to train the computer are fixed, not flexible and shifting physical configurations as happens in real life. To improve their success rate, they ran their predictions through additional machine-learning models that had been trained on data to help them “learn” how proteins and other molecules reconfigure themselves and interact. While this souped-up model got somewhat better results, the researchers report that they still aren’t good enough to identify promising new drugs and their protein targets.
What now? In future studies, the Collins lab will continue to incorporate and train the computers on even more biochemical and biophysical data to help with the predictive process. That’s why this study should be interpreted as an interim progress report on an area of science that will only get better with time.
But it’s also a sobering reminder that the quest to find new classes of antibiotics won’t be easy—even when aided by powerful AI approaches. We certainly aren’t there yet, but I’m confident that we will get there to give doctors new therapeutic weapons and turn back the rise in antibiotic-resistant infections.
By Lawrence Tabak, D.D.S., Ph.D.