Treatment would only be covered for patients enrolled in a clinical trial under the policy, which largely follows a draft proposal released in January.
Medicare will not pay for Biogen's new Alzheimer's medicine unless prospective patients are enrolled in a clinical trial, the U.S. government said Thursday in a decision that will sharply limit the drug's use.
The final policy, issued by the Centers for Medicare and Medicaid Services, largely affirms a draft proposal released in January, which Biogen and its pharmaceutical industry allies had sought to overturn.
In reaching its decision, the agency said the clinical trial data supporting the drug, now known as Aduhelm, were insufficient to conclude that treatment is "reasonable and necessary" — a government standard for coverage.
The policy also applies to other drugs that work similarly to Biogen's if, like Aduhlem, they are approved on the basis of an intermediary measure that predicts, but doesn't prove, clinical benefit.
"We know that there is potential for promise with this treatment," Lee Fleisher, CMS' chief medical officer, said in a call with reporters Thursday. "However, there is not currently enough evidence of clinical benefit to say that it is reasonably necessary for people with Medicare."
The final policy opens the door to somewhat less restrictive coverage should an Alzheimer's drug similar to Aduhelm win approval based on direct measure of clinical benefit. In that case, CMS would cover treatment in approved comparative studies, which may collect data through a registry.
The agency's decision is the latest controversial development for Aduhelm, which received a contentious FDA approval last June. Aduhelm is the first medicine cleared in the U.S. to slow the progression of Alzheimer's disease, rather than temporarily relieve some of its symptoms.
But the evidence gathered by Biogen to support its benefit was contradictory and equivocal, spurring substantial doubt among physicians and even some FDA officials about whether Aduhelm actually helps patients.
When Biogen first looked at data from Aduhelm's main two studies in 2019, it concluded they were likely to fail and discontinued testing. Months later, however, Biogen revisited the data and found signs of benefit in one of the two trials, which it used to apply for Aduhelm's approval.
Independent advisers the FDA later convened were sharply critical of Biogen's results and voted decisively against it. Three members of that committee resigned after the FDA overruled its advice and granted Aduhelm approval.
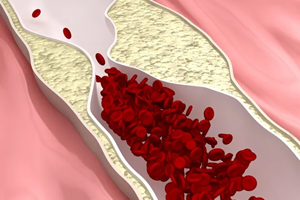
Notably, the FDA approved Aduhelm on an accelerated basis, citing its ability to remove a type of protein called amyloid from the brain. In seeking an OK, Biogen had emphasized data indicating Aduhelm slowed Alzheimer's progression.
Debate among doctors and researchers has simmered since, weighing on Biogen's rollout of the drug, which earned just $1 million in sales over the final three months of last year. That figure was far below what Wall Street analysts had expected, as it's estimated there are roughly 6 million people living with Alzheimer's in the U.S., and treatment options remain limited.
With its finalized policy, Medicare, which covers the largest proportion of Alzheimer's patients in the country, is refusing to cover Aduhelm outside of a strictly managed study, known as a randomized clinical trial.
In a change from the draft, CMS included in its definition any trials cleared by the FDA or run by the National Institutes of Health and removed a requirement that those trials take place in hospitals. For coverage, patients must have mild cognitive impairment due to Alzheimer's disease and evidence of amyloid accumulation in the brain.
Still, the decision will limit Medicare reimbursement for Aduhelm and curtail the market opportunity for experimental Alzheimer's drugs that also target amyloid protein. Three such drugs from Biogen partner Eisai, Eli Lilly and Roche are now in late-stage testing. Lilly recently decided to slow its approval application to the FDA because of CMS' policy.
Should Aduhelm or any of those drugs win full approval based on clinical benefit, CMS policy will allow for slightly broader reimbursement by permitting coverage for patients enrolled in larger, registry-based or "pragmatic" clinical trials.
"This long-term pathway is meant to be nimble and respond to any new drugs in this class that are in the pipeline and demonstrate clinical benefit," said CMS' Fleisher.
Aduhelm's problems have led to drastic action at Biogen. With meager sales numbers and revenue declining from most of its other products, the company in March announced it was beginning layoffs as part of efforts to cut $500 million from its annual spending.
Biogen has yet to disclose specifics on how many or what kind of jobs will be affected. A spokesperson noted to BioPharma Dive in an email last week that the company, as part of the headcount reduction, is prioritizing not filling open positions.
Biogen CEO Michel Vounatsos previously warned of further cost cuts should CMS maintain its draft policy.
In December, Stat News reported that the layoffs would be the biggest in Biogen's history. In 2015, the company laid off about 10% of its workforce as it refocused research around the experimental drug that would become Aduhelm.