The US healthcare industry is massive, with healthcare spending accounting for over 19.7% of US GDP in 2020.
We break down the industry’s various sectors and recent trends hoping to reduce costs while improving care.
The US healthcare industry is massive, and is continuing to grow as the population swells. Many different types of companies and healthcare institutions work together to provide patient satisfaction and a better quality of care—but sometimes it comes at a large cost.
US Healthcare Industry Size & Spending
The global healthcare market will reach $665.37 billion by 2028, according to Verified Market Research. US national healthcare expenditure reached $4.1 trillion in 2020, or $12,530 per person, and is estimated to reach $6.2 trillion by 2028, per the Centers for Medicare and Medicaid Services.
US healthcare is more expensive than most countries. According to the Commonwealth Fund, the US spent nearly 17% of gross domestic product (GDP) on healthcare in 2018. Switzerland was the second-highest ranking country, spending 12.2%. Most surprisingly, New Zealand and Australia devote only 9.3 percent—half as much as the US.
Deloitte estimates that US health spending will balloon from 2020’s $4 trillion estimate to $8.3 trillion by 2040. A main driver of these high costs is healthcare companies’ adoption of emerging health-focused technology. We estimate that US healthcare providers and facilities spent $11.36 billion on cloud-based technologies in 2020—up 33.0% from 2019, when they spent $8.55 billion.
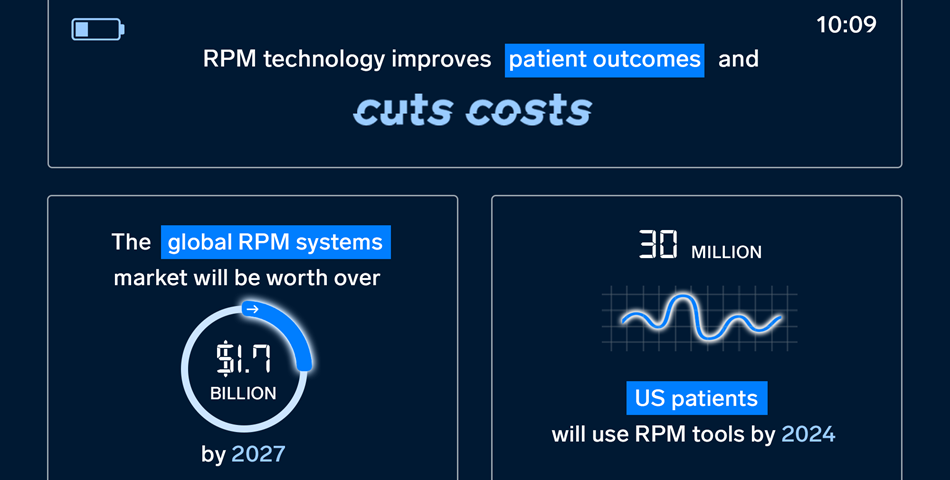
To offset costs, healthcare providers are leveraging the increase in consumers who want to play a more active role in monitoring their own health by encouraging tech that promotes vital tracking, early detection, and prevention of disease. Specifically, remote patient monitoring (RPM) tools, which enable a continuous stream of real-time health data between patients and their doctors, will account for much of this savings.
Considering that 1 in 4 US adults have two or more chronic health conditions, the potential cost savings that can be generated by leveraging RPM technology to avoid unnecessary doctor visits and fees is significant. For example. Medicare’s Chronic Care Management program’s gross savings were $88 million over a 12-month period, generating net savings of $36 million.
Given this impact, other healthcare companies will likely be quick to adopt RPM tech in the future.
US Healthcare Sectors
Healthcare involves many parties working together. From healthcare staffing and administration to providers and patient care, the market is buoyed by a variety of different workers and technologies. Some healthcare sectors include:
- Health insurance
- Healthcare marketing
- Pharmaceuticals
- Healthcare tech
- Health administration
US Healthcare Industry Trends
Traditionally much slower than other industries at adopting digital technologies, healthcare incumbents were finally pushed to digitize everyday systems amid the coronavirus pandemic. The crisis catalyzed a virtual care boom that’s continuing to change the fabric of the entire US healthcare ecosystem.
The digital health industry has been able to react quickly with the help of investors, who’ve been shoveling cash their way: In the first three quarters of 2020 alone, US digital health startups raked in more cash than ever before. Some of the most widely adopted healthcare trends include:
Electronic Health Records (EHRs)
EHRs allow patients’ health information to be managed in a digital format and their data can be shared with other providers across multiple organizations—improving physician productivity and patient satisfaction.
The global Electronic Health Records Market size was valued at $20.55 billion in 2016 and is expected to reach $33.41 billion by 2025, per Markets Insider. And big tech firms like Google and Apple are largely contributing to this growth as they continue to make their way into the digital health market.
Social Determinants of Health (SDOH)
Social determinants of health (SDOH) are non-medical, economic and environmental conditions that both directly and indirectly impact one’s health, like access to transportation and nutritious food.
While care received in medical facilities can account for approximately 10% to 20% of health outcomes, the remaining 80% to 90% can be attributed to SDOH. Last year, 93% of US payers and 95% of US hospitals recorded and took into consideration SDOH when interacting with patients.
Wearables
Wearable technology in healthcare includes electronic devices that consumers can wear, like Fitbits and smartwatches, designed to collect the data of users’ personal health and exercise.
According to our research, the number of health and fitness app users will stay above 84 million through 2022.
Healthcare interoperability
New federal laws and regulations and increase in telehealth brought attention to the lack of interoperability in US healthcare—namely, that payers and providers can’t easily and securely share patient data.
Nearly 59% of doctors believe better interoperability will help them more quickly identify high-risk patients, while 95% of docs agree enhanced interoperability will ultimately improve patient outcomes, per Google Cloud’s July 2021 physician healthcare interoperability survey.